Pelvic Health Physical Therapy: Why Everyone Should See a Pelvic Floor Physical Therapist
In this blog post, we’ll go over everything you need to know about pelvic floor physical therapy, the pelvic floor in general, and how pelvic floor physical therapy can help women who are experiencing pelvic floor symptoms.
Everyone has a pelvic floor, but few know how to relax and lengthen it or do a pelvic floor contraction properly. By learning more about your pelvic floor, you can prevent pelvic floor symptoms and also have a much stronger core.
At Anchor Physical Therapy & Performance, we provide pelvic floor physical therapy for active individuals who like to run, lift weights, do yoga, surf, hike, and many other fun things. I use my pelvic floor rehab training to help my patients draw more awareness to how their pelvic floor integrates with their core and overall movement. This allows my patients to be:
Better movers
Stronger
Confident in their body
Pain free
Reach their goals
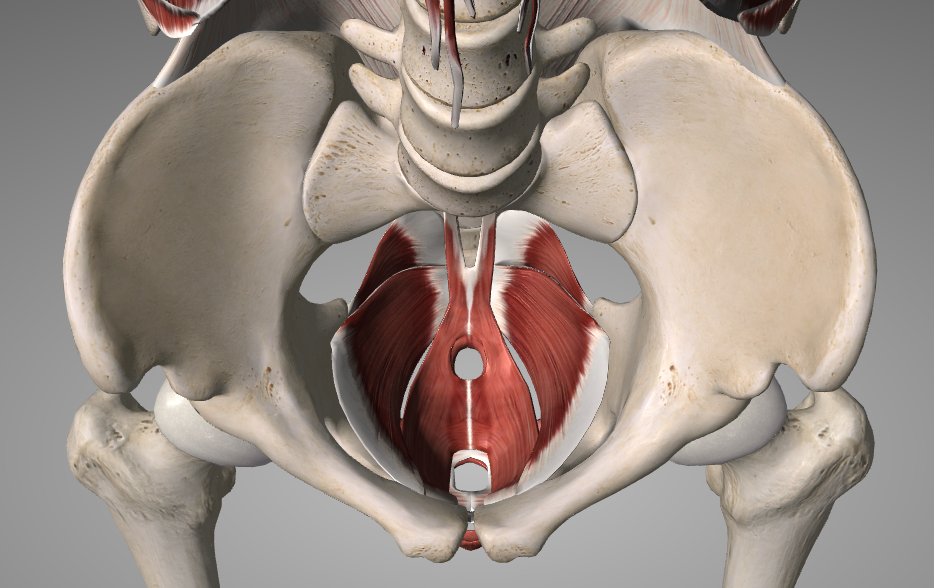
What is the pelvic floor?
The pelvic floor is a group of muscles that lay in the bottom of the pelvis. These muscles contract and relax like any other muscle in our body. Sometimes these muscles can stop working as they should for a variety of reasons. This leads to symptoms such as leaking when you jump or laugh, increased pelvic floor tension, and sometimes pain.
The pelvic floor physical therapist checks if your muscles are strong, tight, or not working well together. This data is combined with the person's overall movement to identify other possible causes of symptoms. From there the root cause can be addressed, a plan is put in place, and you can get back to doing what you love without experiencing pelvic floor symptoms.
The importance of pelvic floor health for women
Understanding how the pelvic floor works helps many women avoid unwanted symptoms and can prevent pelvic health issues. We can also support and protect the hips, lower back, and core which can help reduce orthopedic problems such as hip and lower back pain in the future.
You may have heard of Kegal training. But Kegels are not the only way to manage pelvic floor symptoms and dysfunction. Plus.. most people are not doing pelvic floor contractions (or kegels) correctly. Unfortunately, this is the only education that is often given to women by other medical providers. Doing a pelvic floor contraction incorrectly and managing intra-abdominal pressures incorrectly can lead to:
Pelvic pain
Pelvic floor tension
Urinary incontinence (leaking urine- even just a few drops counts!)
Fecal incontinence
Constipation
Pelvic floor heaviness
Pubic symphysis dysfunction (pain on the pubic bone)
Sacroiliac joint (SIJ) pain
How many people have pelvic floor dysfunction?
Pelvic floor dysfunction is extremely common, but does not have to be accepted as a new normal.
Here are some statistics from a self reported study for urinary incontinence incidence rates. This is really high, and does not have to be the case (1).
25% of young women
44-57% of middle-aged women and postmenopausal women
75% of older women in nursing homes
(Urinary Incontinence New Hope, 2012)
These symptoms can greatly impact daily life and recreation. It is ideal for everyone to work on prevention. If you are someone experiencing these symptoms already, it is never too late to address it with a pelvic floor physical therapist. So much can be done to help the pelvic floor muscles relax, and strengthen in order to reduce your symptoms and get you back to your prior level of activity.
How does pelvic floor dysfunction happen in the first place?
The pelvic floor is one part of our core stabilization system. The other parts include the diaphragm (how we breathe), the abdominal muscles, and the lower back muscles. These 4 components make up the core canister (think of a soda can). When one part of this canister is too tight or produces more force than the other parts of the canister, the soda can bend or protrude in different areas to compromise.
Ways that pelvic floor symptoms can develop:
Heavy weight lifting with poor pressure management (creating pressure down on the pelvic floor)
Running with faulty mechanics (potentially)
Poor breathing mechanics which put more pressure on the pelvic floor
Lower body weakness that reduces our body’s ability to absorb shock
High stress/anxiety leading to chronic pelvic floor tension
Poor bladder habits
Poor postures that involve glute or abdominal clenching (increasing tension to the pelvic floor)
Aging: hormone and connective tissue changes
Major pelvic floor events such as pregnancy/labor/delivery
Over time, these small pressure changes in our body can lead to a tight or weak pelvic floor that has difficulty functioning as it normally should.
It is never too early to educate yourself on how your pelvic floor functions and how it relates to the rest of the body.
It is my belief that all women should see a pelvic floor physical therapist.
What is Pelvic Floor Physical Therapy
The goal of a pelvic health physical therapy session is to determine where the source of your symptoms are coming from and how the pelvic floor is playing a role in your movement patterns. Pelvic floor rehab can be performed by other trained medical professionals such as occupational therapists and nurse practitioners.
A typical pelvic floor evaluation would consist of:
Full body movement screen- determining if there are other parts of the body that are contributing to pelvic floor dysfunction
Functional movement assessments- watching you perform the activity that is causing you symptoms (running, lifting your baby, etc)
Strength testing- often assessing core and hip strength
Pelvic alignment assessment - is the pelvis rotated causing some asymmetry in your body?
External pelvic floor and hip assessment: feeling for any trigger points that may be contributing to symptoms
Internal pelvic floor examination- often required to determine if the pelvic floor is tight, weak, or not coordinating well
Manual therapy and sometimes dry needling if applicable
Once the source of the problem has been identified, the physical therapist will come up with a treatment plan to address the root cause of your symptom complaint. This often consists of:
Education: learning about pelvic floor anatomy, bladder health, bowel/digestive health, and stress management strategies are all essential to include in pelvic floor treatment
Pain relief: if pain is part of your journey, then anything I can do to relieve those symptoms is a top priority (joint mobilizations, deep tissue work, cupping, dry needling, taping, etc)
Breathwork: training the body to utilize a 360 breathing pattern allows the pelvic floor to relax and contract as it should
Pelvic floor relaxation: learning how to release tension in the pelvic floor so it has the ability to work through its full range of motion
Pelvic floor connection and strengthening: learning how to correctly perform a PF contraction and activate the deep core stabilizing muscles
Corrective movement exercises: connecting the pelvic floor to how we move on a daily basis so results will last longer
Functional strength training: everyone needs to be strong, whether it is lifting groceries or a car seat
Why it's essential to learn about your pelvic floor
Pelvic floor physical therapy gives women a lot of information about their body that you would not know without a trained professional. If you learn how your body manages pressure, or where your body holds tension, it can guide you on different exercises you should do more of, positions you should spend less time in, etc. If you have this education, you will know how to manage your symptoms independently. Learning about your pelvic floor health can prevent future UTIs, prolapse, incontinence, pelvic pain, and more.
Common Pelvic Health Issues for Women
Pregnancy-related symptoms:
There are many postural and hormonal changes that happen over the course of pregnancy. While this is all part of the exciting journey to motherhood, it can also cause pressure changes within our core that can be challenging to manage. Common symptoms related to pregnancy include:
Pubic symphysis dysfunction (SPD) - pain in the front of your pubic bone
Sacroiliac joint (SIJ) pain - one-sided pain in the lower back/upper glute region
Low back pain
Hip pain
Foot/ankle pain
Round ligament pain - pain in the low abdomen as your uterus is growing
Upper back/shoulder blade pain
Urinary incontinence (leaking)
Understanding how the pelvic floor works can help lead to a more comfortable pregnancy, empower you for your delivery, and expedite your postpartum recovery. If you are looking to strengthen your pelvic floor for labor visit our Third Trimester Exercises to Prepare for Labor blog.
Postpartum rehab
In the postpartum period, we are left with a whole new body that can be very challenging to reconnect to. During the first few weeks, your body needs to rest and heal from the act of carrying a baby to term and the healing of the labor and delivery.
The abdominal muscles separate on all pregnant women to make space for the baby, and for some, the abdominal muscles have a harder time “closing”. This is called diastasis recti and can be treated through pelvic floor physical therapy (3).
It is so important for all postpartum women to reconnect to their deep core stabilizing muscles, pelvic floor, and breath.
This may sound self-explanatory, but most people have a hard time doing these things in general and usually need guidance from a trained professional. Everyone will need different things (more muscle engagement, more muscle relaxation, more breath work, more conditioning), and the list goes on. Urinary incontinence is common to occur due to the strenuous nature of labor and delivery. Vaginal deliveries are twice as likely to have incontinence issues vs. cesarean delivery (4).
It is important to get a full body movement analysis performed so you know what exercise program would work best for you in your new body. Even just one pelvic floor physical therapy session can be hugely impactful in your life.
Pelvic floor physical therapy is something all postpartum women should do, no matter how their pregnancy went, whether they are strong or not, or whether they were in pain or not.
It is all about how you are utilizing your breath and core to manage pressures in daily life. If you address this early on you can prevent issues in the future, and feel more connected, feel strong, and get back to the activities you enjoyed prior to pregnancy.
Being a parent is also very physical and involves a lot of forward posture. This can cause a variety of other pains in the body that can greatly impact your life as a parent. Anchor Physical Therapy & Performance can address all orthopedic aches and pains that come along with early motherhood. Common symptoms I hear from postpartum women are:
Shoulder pain
Thumb pain
Upper back/shoulder blade pain
Low back pain
Menopause-related changes
Menopause is a cascade of hormonal changes that all women will experience at some point. This has impacts on many parts of your body, some of which are well known (your skin, how you carry your weight, etc). But menopause can also cause a lot of bladder changes. The change in hormones causes a different climate in your bladder that can cause urinary urgency (feeling like you can’t hold your bladder as long as you would like), increase in frequency (feel like you go to the bathroom all of the time), and stress incontinence (peeing a little bit when you sneeze, laugh, etc). Part of this is due to the change in connective tissue that can cause the pelvic muscles to have less tone and less fascial pull to hold organs up. This can cause pelvic organ prolapse or falling. Society tends to accept these changes as a part of aging with no solution. What I wish more people knew was that pelvic floor physical therapy can help menopausal women with many of these symptoms by learning about bladder health, reconnecting with their core, and restoring mobility.
Pelvic Floor Physical Therapy and Urinary Urgency or Frequency
Increased urinary frequency can occur due to something as simple as bad habits of going to the bathroom more than you need to. This can progress to the point where your bladder has the inability to hold your urine for long periods of time. Other factors that contribute to urinary urgency and frequency are a tight pelvic floor, a weak pelvic floor, or poor pelvic floor muscle coordination. Certain bladder irritants such as coffee or alcohol can further contribute to symptoms.
Stress incontinence (Leaking of urine)
Stress incontinence is when the pelvic floor has a hard time maintaining tension to hold urine in during times of stress. This includes leaking with sneezing, laughing, coughing, jumping, or running. This is a very common complaint among women and can be changed no matter how long symptoms have been going on. Addressing full body mechanics with running and jumping can make a big difference with stress incontinence. Pelvic floor tension is also a very common cause for leaking with activity and can be addressed with the right exercises and treatment.
If this sounds like you, visit our blog on 5 Steps to Improving Bladder Control.
Pelvic organ prolapse (POP)
Pelvic organ prolapse is when the pelvic organs start to protrude into the vaginal canal. Symptoms commonly described are pelvic floor “heaviness” and sometimes feeling like you are “sitting on a ball”. There are different grades of prolapse from a slight protrusion into the wall to the organs moving completely out of the body. This is commonly seen in postpartum women at any age, due to the amount of pressure placed on the pelvic floor during pregnancy and labor/delivery. In menopause the natural fascial tension we have holding the pelvic organs up starts to loosen, increasing the likelihood of POP. I also see prolapse in individuals who have never been pregnant, and this is typically due to altered breathing and pressure of the core canister leading to abnormal pressure down on the pelvic floor. If you think you might be suffering from pelvic floor prolapse, check out our blog How do I know if I have prolapse? While prolapse sounds scary, it is extremely common and there are many things that can be done to help reduce the degree of prolapse. There are also exercises that can be done to help restore normal pressure and tension around the pelvic floor to prevent it from getting worse in the future (5).
Types of pelvic organ prolapse:
Cystocele (anterior vaginal wall collapse) - when your bladder protrudes into the vaginal canal
Rectocele (posterior vaginal wall collapse) - when your rectum protrudes into the vaginal canal
Uterine prolapse - when your uterus descends into the vaginal canal
Constipation
The inability to have regular bowel movements is something that many people experience and can impact a lot of other systems in the body. Constipation is impacted greatly by the food you are putting into your body, so working with a dietician can be very helpful to get guidance on this. But there are a lot of lifestyle changes that can be worked on in pelvic floor physical therapy to help with increasing the quality and frequency of your bowel movements.
Common physical therapy interventions I work on to help with constipation:
Squatty potty: a tip for all people to have easier bowel movements
Pelvic floor release: manual work or home exercises to improve ease of bowel movements
Effective pushing techniques: are you actually being productive when you push?
Self massage techniques that can help encourage a bowel movement
Breath work - the diaphragm helps mobilize the bowels
Diet and lifestyle modifications: are you taking your time to eat? Do you chew your food enough?
Pelvic pain or pain with intercourse
Women can experience all different types of pain located in the pelvic region. Often it can be from trigger points in the pelvic floor, general pelvic floor tension, or potentially a referral of pain coming from a different part of the body. This pain can be severe and chronic for some people, and often there are solutions to this pain by finding the right exercises or manual releases in pelvic floor physical therapy. Pelvic tension can cause intercourse to be very challenging and painful. Addressing the reason behind your pain and working on finding the right sex position and/or the right exercises to do before sex can make a huge impact in your pain and sex life.
How Exactly Pelvic Floor Physical Therapy Can Help Women
It doesn’t matter how old you are, how long your symptoms have been around for, pelvic floor physical therapy can absolutely help you reach your goals. Even if someone is unsure if they have a pelvic floor dysfunction or not, it is very empowering to just learn more about how your pelvic floor works, and how it connects to the rest of your body.
Each patient is looked at as an individual, and what specific goals you have. If at any point a part of treatment doesn’t feel right for you, we can modify and focus on what does feel most helpful for you.
Pelvic Floor Physical Therapy Services at Anchor PT in Portsmouth, New Hampshire
At Anchor Physical Therapy & Performance, I help women achieve their physical fitness goals by integrating pelvic floor health. I believe all people can benefit from pelvic floor physical therapy to improve their connection and understanding to how the pelvic floor works in relation to our core, hips, low back, and upper body.
As a society it can be uncomfortable to talk about the pelvic floor, so therefore it is avoided completely. Women are out there running, lifting heavy weights, and having babies without having an understanding of what is happening in their pelvic floor. It is my goal to educate everyone about their core and pelvic floor so we can all be strong, and have healthy pelvic floors for the rest of our lives.
The population I enjoy working with the most is postpartum women who are trying to get back to working out. Partly because I lived it myself, and have become passionate about making sure postpartum women fully rehabilitate prior to getting back to their higher level activities such as running, lifting, skiing, etc.
Patient testimonials and success stories.
“I cannot recommend Lauren enough! I was apprehensive about seeking out help with pelvic floor therapy for DR [diastasis recti] after having a child. Working with Lauren I quickly learned how much more of the body is related, the Core is involved in everything. She is an incredibly knowledgeable and thoughtful provider, you truly work as a team. I have a stronger core and back(and whole body really) now and less discomfort than I have in many years. She is my go to for top quality physical therapy!”
—Michelle
“I was lucky to find Lauren post-pregnancy and multiple surgeries to help me regain functional movement, reduce back pain, and improve some nerve issues. Her knowledge in the field is truly impressive…. Lauren helped quickly get my functional movement back, but also provided me with valuable guidance and exercises for long-term maintenance.
If you're in need of a pelvic floor or orthopedic physical therapist who combines extensive knowledge with a client-centered approach- Lauren is the physical therapist for you!”
—Christine
The Many Benefits of Pelvic Floor Physical Therapy for Women
Improved quality of life
Improved connection with your deep core to feel more confident in workouts and fitness
Lift heavier weights by having better intra-abdominal pressure
Enhanced postpartum recovery
Prevent other orthopedic related issues that can arise due to pelvic floor dysfunction (low back pain, hip pain, etc)
Reduce the aches and pains of common pregnancy symptoms
Prepare for labor and delivery
Optimize your pelvic health for conception and future pregnancy
Improved bowel movement quality and frequency
Control bladder leaks with jumping, running, laughing, sneezing, and coughing
Reduced stress and anxiety by addressing breathing patterns and pelvic floor tension
Preventing incontinence, prolapse, and other pelvic floor dysfunction in the future
Supports sexual health
Stay out of nursing homes longer
Why You Should Schedule An Appointment Today
The New Hampshire seacoast is an active community, and nothing is more annoying than having a pelvic floor dysfunction holding you back from doing what you love. Learning more about your pelvic floor and how to connect it to your breath and core helps prevent so many pelvic related complaints in the future. If you are an active person, you need to understand this connection even more. Start your journey to feeling more empowered about your pelvic floor and how you move as a whole by making your first appointment with Anchor Physical Therapy & Performance in Portsmouth, NH today.
References mentioned in this blog post:
Urinary Incontinence New Hope: Research Activities, July 2012, No. 383. Agency for Healthcare Research and Quality, Rockville, MD. Retrieved July 2012 from https://archive.ahrq.gov/news/newsletters/research-activities/jul12/0712RA3.html
Wallace SL, Miller LD, Mishra K. Pelvic floor physical therapy in the treatment of pelvic floor dysfunction in women. Current Opinion in Obstetrics and Gynecology. 2019;31(6):485-493. doi:https://doi.org/10.1097/gco.0000000000000584
Kepenekci, M.D I, Keskinkılıc, M.D. B, Akınsu, M.D. F, et al. Prevalence of Pelvic Floor Disorders in the Female Population and the Impact of Age, Mode of Delivery, and Parity. Diseases of the Colon & Rectum . 2011;54(1):85-94. doi:https://doi.org/10.1007/DCR.0b013e3181fd2356
Tähtinen RM, Cartwright R, Tsui JF, et al. Long-term Impact of Mode of Delivery on Stress Urinary Incontinence and Urgency Urinary Incontinence: A Systematic Review and Meta-analysis. European Urology. 2016;70(1):148-158. doi:https://doi.org/10.1016/j.eururo.2016.01.037
Hoff Brækken, PhD, PT I, Majida, MD M, Ellström Engh, MD, PhD M, Bø, PhD, PT K. Can pelvic floor muscle training reverse pelvic organ prolapse and reduce prolapse symptoms? An assessor-blinded, randomized, controlled trial. American Journal of Obstetrics & Gynecology. Published online February 15, 2010:1.e1-1.e7. doi:https://doi.org/10.1016/j.ajog.2010.02.037